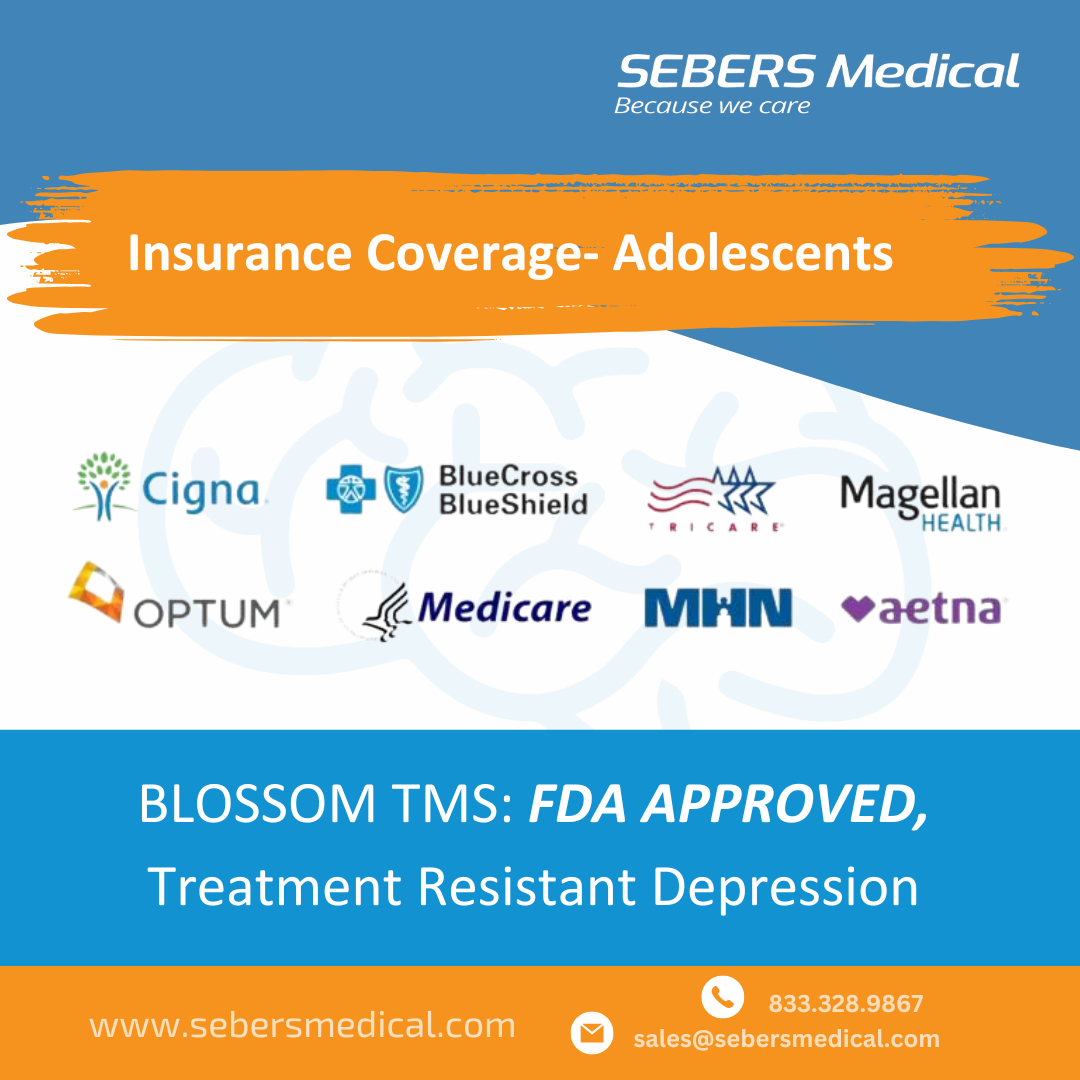
Transcranial Magnetic Stimulation (TMS) is now available for adolescents as young as 15, and insurance providers like Aetna are expanding their coverage to meet this growing demand. As of now, Aetna has updated their policies to cover TMS for adolescents aged 15 and older with Major Depressive Disorder (MDD), but this shift is likely to inspire other insurance companies to follow suit.
Key Points from Aetna’s TMS Coverage Policy:
- Eligibility: Adolescents aged 15 years and older with MDD are eligible for TMS treatment under Aetna’s coverage.
- FDA-Cleared Devices: Aetna’s guidelines specify that any FDA-cleared TMS device can be used for treatment, meaning that providers using the Blossom TMS device can confidently offer this service to adolescent patients.
Are Other Insurance Providers Following?
While Aetna is a leader in expanding adolescent TMS coverage, many other insurance providers are likely to follow this trend. Given the effectiveness and growing recognition of TMS as a non-invasive treatment for MDD, it’s expected that other insurers like Humana and BlueCross BlueShield may soon update their policies to include adolescent coverage as well.
What Should Providers Do?
For clinics and providers, the best practice is to check directly with insurance companies regarding their specific coverage for adolescent TMS. Since each insurance provider has its own set of guidelines, verifying coverage before initiating treatment is key to ensuring the best possible care for patients.
Conclusion
The expansion of TMS coverage for adolescents marks a significant step forward in treating mental health conditions in younger populations. As more insurance companies update their policies, TMS will become even more accessible, allowing more adolescents to benefit from this life-changing therapy.
If you want to learn more about how Blossom TMS can help adolescents, visit our blog or contact us today.
Source: https://www.aetna.com/cpb/medical/data/400_499/0469.html